Lymphoedema
Causes of limb swelling
Bilateral pitting oedema
- Heart failure
- Renal disease
- Proteinuria
- Cirrhosis
- Carcinomatosis
- Nutritional
Painful unilateral pitting oedema
- Deep venous thrombosis
- Superficial thrombophlebitis
- Cellulitis
- Trauma
- Ischaemia
Painless unilateral oedema
- Post-phlebitic limb
- Extrinsic compression of the deep veins
- Deep venous incompetence
- Lymphoedema
- Immobility
Lymphoedema
- Lymphoedema presents with gradual limb swelling
- Due to progressive failure of lymphatic system
Primary lymphoedema
- Congenital (age < 1 year) - familial or non-familial
- Praecox (age < 35 years) - familial or non-familial
- Tarda (age > 35 years)
Secondary lymphoedema
- Malignant disease
- Surgery - axillary surgery or groin dissection
- Radiotherapy
- Infection - parasitic (e.g. filariasis)
Pathology
- Primary lymphoedema is the result of a spectrum of lymphatic disorders
- Can be due to aplasia, hypoplasia or hyperplasia of lymphatics
- In 80% obliteration of distal lymphatics occurs
- A proportion of patients have a family history (Milroy's disease)
- In 10% proximal occlusion of lymphatics in abdomen and pelvis is seen
- In 10% lymphatic valvular incompetence develops
- Chronic lymphoedema results in subcutaneous fibrosis
- Fibrosis can be worsened by secondary infection
Clinical features
- The initial presentation is usually with peripheral oedema worse on standing
- Begins distally and progresses proximally
- Limb usually feels heavy
- Can be unilateral or bilateral
- Primary lymphoedema is more common in women and is usually bilateral
- With secondary lymphoedema the underlying cause if often apparent
- Examination shows non-pitting oedema
- The skin often has hyperkeratosis, fissuring and secondary infection
- Ulceration is rare
Investigations
- Chronic venous insufficiency should be excluded with doppler ultrasound
- Lymphoedema and its cause can be confirmed with
- Lymphoscintigraphy
- CT or MRI scanning
- Lymphangiography
- Lymphoscintigraphy is usually the investigation of choice
- Has a sensitivity > 90% and specificity of 100%
- Normal lymphoscintigraphy excludes a diagnosis of lymphoedema
- Lymphangiography is painful and rarely required
Management
- The aims of treatment are to
- Reduce limb swelling
- Improve limb function
- Reduce the risk of infection
Conservative treatment
- General skin care will reduce risk of infection
- Swelling can be reduced by elevation
- Physiotherapy and manual lymph drainage may help
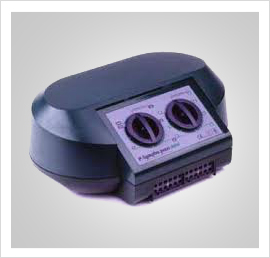
- External pneumatic compression will also reduce swelling
- Once swelling is reduced compression stockings should be applied
- Antibiotics should be given at the first sign of infection
- Drugs (e.g. diuretics) are of no proven benefit
Surgery
- Surgery consists of two approaches
- Debulking operations
- Bypass procedures
- Debulking operations include
- Homan's operation - elliptical excisions of skin and subcutaneous tissue with primary closure
- Charles' operation - radical excision of skin and subcutaneous tissue with skin grafts
- Both produce good functional results
- Cosmesis is often poor
- Bypass operations include:
- Skin and muscle flaps
- Omental bridges
- Enteromesenteric bridges
- Lymphaticolymphatic anastomosis
- Lymphaticovenous anastomosis
Dr. Pankaj Patel a vascular surgeon has expertise in peripheral vascular diseases, varicose veins and deep vein thrombosis